Swan-Ganz catheter
The Swan-Ganz catheter is a pulmonary artery catheter frequently used for right heart catheterization to evaluate heart failure, abnormalities and valve function. This catheter was designed by Dr. H.J.C. Swan and Dr. William Ganz who gave their contributions to the pulmonary catheter by adding an inflatable balloon tip to facilitate advancement of the catheter into the pulmonary artery. The second modification to the pulmonary catheter was the addition of a thermistor to measure cardiac output.
The most basic Swan-Ganz catheter is shown in the diagram above. The catheter contains multiple lumens allowing pressure measurement, blood sample collection, and pharmacologic administration. Each lumen is connected to a port.
The distal port continues the entirety of the catheter and exists at the tip. The port is used to evaluate the pulmonary arterial pressure and pulmonary capillary wedge pressure. A 0.025 inch wire can be inserted into this port to assist in advancing the catheter into the pulmonary artery. Mixed venous blood samples can be obtained from this port.
The proximal port continues through the catheter and has an exit port approximately 26 cm from the tip. This location is closely approximated to the right atrium and can be used for central venous pressure assessment, medication and fluid administration, and thermodilution cardiac output injections.
The thermistor connector is connected to a monitor to display internal temperature readings. These temperature readings are important for cardiac output measurements. The thermistor itself is located just proximal to the balloon at the distal tip of the catheter. Cardiac output is measured when cool injectate is delivered rapidly into the proximal port and the change in blood temperature is plotted over time until return to normal.
The balloon syringe allows for inflation of the balloon to help facilitate catheter advancement to the pulmonary artery. The balloon is inflated with less than 1.5 mL of air. The balloon is deflated once the catheter is positioned in the pulmonary artery. To obtain a wedge tracing, the balloon is then reinflated to wedge the catheter into a distal pulmonary artery.
SGC Insertion
- After the introducer sheath is inserted into the vein, the SGC can be inserted through the introducer and advanced toward the right atrium.
- The SGC balloon can be inflated with the 1.5ml syringe to allow for flow mediated advancement and to prevent myocardial or valvular injury. Inflate slowly! A small amount of resistance is normal, but excessive resistance requires repositioning of the catheter.
- In the Cardiac Cath Lab, the SGC is usually advanced under fluoroscopy. Keep in mind that the catheter also has markers every 10cm and that understanding the physiologic "rule of 10s" will also help in understanding where the SGC should be positioned.
- Once in the right atrium, the SGc is rotated to advance over the tricuspid valve into the right ventricle.
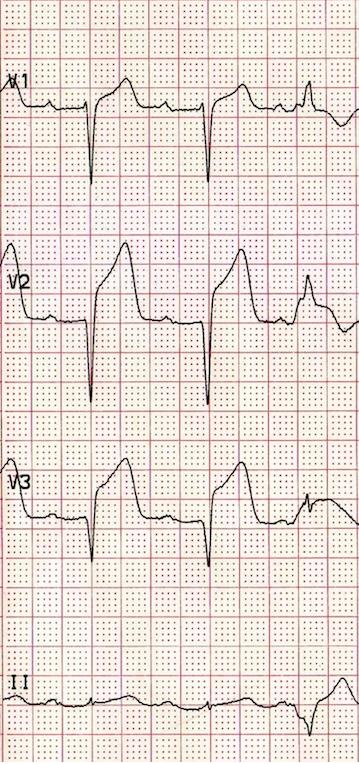
- Be aware that ventricular arrythmias may occur from catheter stimulation. The SGC is rotated upward and advance over the pulmonic valve and into the pulmonary artery.
- Dilated right atriums, and pulmonary valve complications may make advancing the SGC into the pulmonary artery a challenge. A 0.025 wire may be inserted into the SGC to assist in advancing the catheter.
- Once in the pulmonary artery, the catheter should be advanced until pulmonary capillary wedge pressure is identified. The balloon should then be deflated. Check waveform for a return to pulmonary artery waveform, otherwise the catheter should be withdrawn until correct waveform is identified.
- Pull back on the SGC to minimize the slack that may exist in the right ventricle. This will minimize ventricular ectopy and allow for the proximal port to be positioned near the right atrium.