Bare Metal Stents
A stent is a tube shaped device placed in an artery to expand a blocked region to improve blood flow through the artery. A bare metal stent (BMS) is a stent without any drug coating. The first stents were made of stainless steel. Modern stents are made using a cobalt chromium allow or a platinum chromium allow to decrease the bulk size of the stent while providing increased strenght.
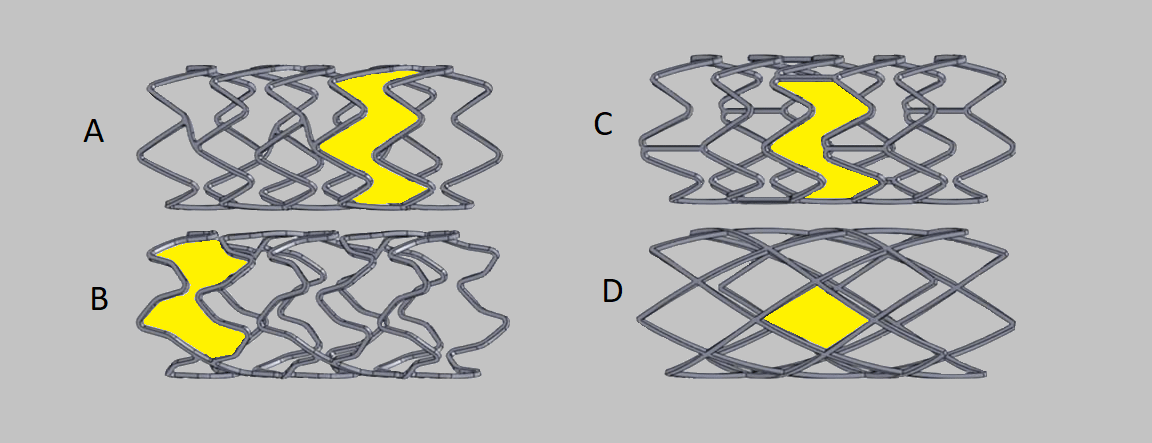
Stents come in a variety of patterns as noted in the image above. Some consideration with the design of stents include patterns that provide strong radial force to maintain the integrity of the inflated stent while also providing flexibility to accomodate delivery of the stent into the tortuous anatomy of the coronary artery. The shaded regions in the above images represent the cell space of the stent. Larger areas of cell space are known as open cell and are more flexible for delivery but can present with higher rates of restenosis in those areas. The smaller closed cell are not as easily deliverable but do provide better coverage of the blocked area.
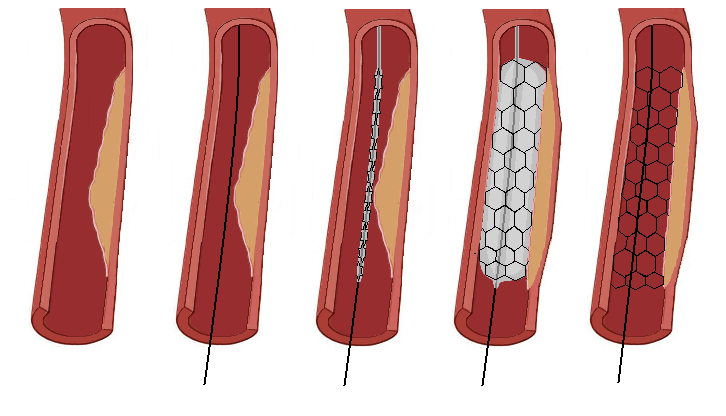
When a stent is inserted into the atery and expanded in the region of a blockage, the procedure is known as "direct stenting". Some blockages may be too complicated to allow for direct stenting. When this occurs, balloon angioplasty may be required to predilate the blockage to allow the insertion of the stent. The stent is deployed in the same fashion as balloon angioplasty. When the stent platform is expanded, the balloon will expand the crimped stent to the edges of the arterial wall. The balloon is then deflated leaving the stent in place. The balloon platform is then pulled back into the guide catheter so that post stent dilation can be visualized for proper placement. Additional customization of the stent may be required to expand regions of the stent with non-compliant balloons to make sure the stent is fully deployed and match the proximal and distal segments of the artery.
Complications with Stenting
- Restenosis is the renarrowing of the artery due to immune responses to the foreign material. After stent deployment, cell proliferation will occur to cover the stent. Smooth muscle tussue may also develop at the stented region and can be severe enough to occlude the artery. One of the major contributors to restenosis is a stent that is undersize and not fully deployed against the walls of the artery.
- Thrombosis occurs when clots form at the site of stent where the arterial wall is damaged from expansion during angioplasty. Antiplatelet therapy will help to minimize the roll of platelets to form a blood clot at the region of the stent until the artery forms a natural smooth layer of cells over the stent. Aspirin is a common antiplatelet drug used post stenting. Dual antiplatelet therapy will combine Aspirin with Clopidogrel (Plavix) or Ticagrelor (Brilinita) for up to a year or longer post stent placement.
- Dissection occurs when the inner lining of the arterial wall splits or tears away form the atery. This is visualized as a haziness and or flap appearance during the post stent imaging. The dissected region compromises blood flow through the artery and must be treated before it lengthens and causes critical compromise of the artery. Treatment involves additional stenting along the dissected region
- Plaque Shifting occurs when the plaque material underneath the intimal layer of the artery shifts past the stented region. Additional stenting may be required if the shifting is noticibly compromising blood flow through the artery.
Prep the Stent
- Carefully remove and inspect the stent/balloon catheter from the package.
- Attach a stopcock to the catheter inflation hub.
- Attach a syringe of 50% solution of contrast and heparinized saline to the stopcock.
- Open the stopcock and pull back negative pressure with the syringe.
- Carefully release the negative pressure allowing the balloon catheter to pull in the solution.
- Close the stopcock to the balloon catheter and purge any air out of the syringe.
- Repeat steps 4 to 6 a few times as necessary to remove air from the catheter.
- Carefully remove the stylet and stent/balloon cover from the catheter tip.
- Use the flushing needle and a syringe to flush the distal tip of the catheter with heparinized saline.
- Submerge the catheter in heparinized saline to activate any hydrophilic coating on the shaft of the catheter.
References
- Baim, D.S. (2005) Grossman's Cardiac Catheterization, Angiography, and Intervention. (7th ed.). Philadelphia,Pa: Lippincott, Williams & Wilkins.
- Kern, M. et al (2003) The Cardiac Catheterization Handbook (4th ed.). Philadelphia, Pa: Mosby.