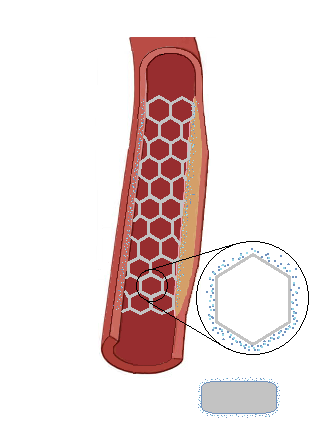
Drug Eluting Stents
A drug eluting stent (DES) is a stent that slowly releases a drug to prevent rapid cellular reproduction called proliferation at the site of the stent. When the endothelial cells of the lining of the coronary artery become damage, the cells will proliferate to create a new layer over the damaged artery wall. Somestimes this process can aggressively repeat itself until the artery becomes blocked again. DES have significantly reduced restenosis after angioplasty and have been shown to be statistically superior to bare metal stents. The stent contains a layer of polymer that helps hold and release the drug once deployed against the arterial wall. Medications used with DES included immunosuppressive and antiproliferative drugs that included Sirolimus or Paclitaxel.
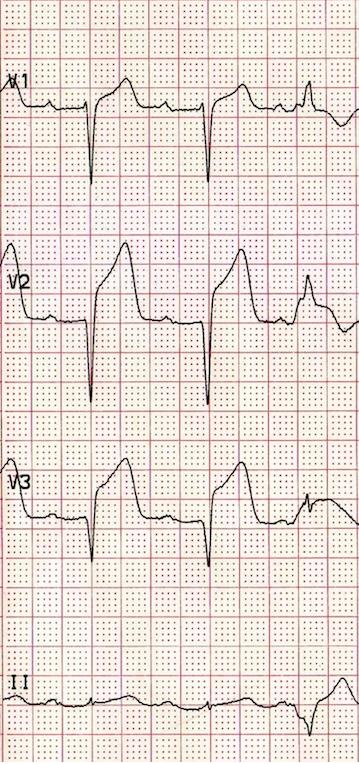
Complications with DES Stenting
- Restenosis is significantly decreased with DES but can occur. When restenosis occurs, it is important to consider the cause of restenosis, such as underdeployment, or use a DES with a different drug on it.
- Thrombosis occurs when clots form at the site of stent where the arterial wall is damaged from expansion during angioplasty. Antiplatelet therapy will help to minimize the roll of platelets to form a blood clot at the region of the stent until the artery forms a natural smooth layer of cells over the stent. Since DES will be exposed to blood flow longer than a BMS, antiplatelet therapy will need to be established longer than before. Aspirin is a common antiplatelet drug used post stenting. Dual antiplatelet therapy will combine Aspirin with Clopidogrel (Plavix) or Ticagrelor (Brilinita) for up to a year or longer post stent placement.
- Dissection occurs when the inner lining of the arterial wall splits or tears away form the atery. This is visualized as a haziness and or flap appearance during the post stent imaging. The dissected region compromises blood flow through the artery and must be treated before it lengthens and causes critical compromise of the artery. Treatment involves additional stenting along the dissected region
- Plaque Shifting occurs when the plaque material underneath the intimal layer of the artery shifts past the stented region. Additional stenting may be required if the shifting is noticibly compromising blood flow through the artery.
Prep the Stent
- Carefully remove and inspect the stent/balloon catheter from the package.
- Avoid contactacting the stent with any fluid to avoid the initiationof drug release.
- Attach a stopcock to the catheter inflation hub.
- Attach a syringe of 50% solution of contrast and heparinized saline to the stopcock.
- Open the stopcock and pull back negative pressure with the syringe.
- Carefully release the negative pressure allowing the balloon catheter to pull in the solution.
- Close the stopcock to the balloon catheter and purge any air out of the syringe.
- Repeat steps 4 to 6 a few times as necessary to remove air from the catheter.
- Carefully remove the stylet and stent/balloon cover from the catheter tip.
- Open stockcock to stent delivery system and prepare for insertion.