Radiation
All professionals in the cardiac cath lab have voluntarily accepted some degree of radiation exposure, but they are obligated to minimize and reduce risks to other personnel, themselves and their patients. Radiation is invisible and can easily be ignored, but it should be respected.
X-ray is a form of electromagnetic radiation. With its very short wavelength and very high frequency, each x-ray photon can pass through solid matter and captured to film or monitor. These characteristics also explain why different and more potent biologic effects occur when an x-ray photon is absorbed or scattered from living tissue.
X-ray dose and measurement Important radiation safety programs must manage patient and staff safety by reducing exposure to x-ray to a level that is as low as reasonably achievable (ALARA). X-ray dose measurement can be seen by the following:
Fluoroscopic time (FT) is the time during a procedure that fluoroscopy is used. Since FT does not include cine acquisition imaging, it is not a useful descriptor of patient radiation dose.
Total air kerma (AK) at the interventional reference point is the procedure cumulative x-ray energy delivered to air at the interventional reference point. It is used to monitor patient dose as it is associated with deterministic skin effects, though it is not the true peak skin dose.
Air kerma area product (PKA, Gy/cm2) is the sum of the product of instantaneous air kerma and x-ray field area. It is comonly reported by modern systems and is used to monitor patient dose and possible risk of radiation induced cancer.
Peak skin dose (PSD, Gy) is the maximum dose received by any local area of patient skin. When PSD increases, the probability and severity of deterministic skin effects increase. PSD is estimated by air kerma and x-ray geometry details.
Scattered Radiation is produced when the x-ray beam interacts with the patient and is redirected rather than absorbed completely. If scattered radiation reaches the image receptor, it contributes to noise and reduces the image contrast created as the primary x-ray beam interacts with the anatomic structures. Scatted radiation is also the principal source of exposure for the patient's body parts that lie outside the field of the primary x-ray beam and also for the staff. The amount of scatter increases with increases in the intensity of the x-ray beam and the size of the x-ray field.
Radiation production and control
Generators The cinefluorographic x-ray generator controls and delivers electrical power to the x-ray tube. It heats the x-ray tube's filament to produce a beam of electrons that are accelerated toward the target anode. The flow of high-energy electrons toward the anode is not continuous, but is separated into 15 to 60 pulses per second (pulsed fluoroscopy).
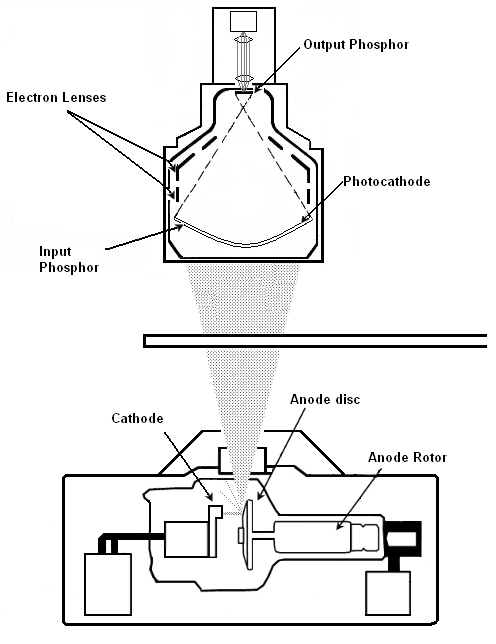
X-ray tubes The x-ray tube is a device that converts a portion of the electrical energy delivered by the generator into x-rays. The x-ray tube consists of an evacuated glass or metal housing that contains a tungsten filament, and an anode disc, which rotates at more than 10,000 rpm. Electrons are emitted from the filament and accelerate toward the anode under the influence of the electric field supplied by the generator.
Imaging Modes
fluoroscopy provides a real-time x-ray image for guiding manipulations. This allows significantly lower x-ray input doses than those needed for acquisition. Many systems offer variable fluoroscopic frame rates. Decreasing the frame rate saves dose at the expense of visual smoothness of the transition between frames. Many operators find 15 frames per second (fps) to be satisfactory for digital cardiac fluoroscopy.
acquisition/cine generates images of sufficient quality for singe-frame viewing. Higher x-ray input dose rates are needed to reduce image noise and optimize visualization with a per-frame dose approximately 15 times greater than fluoroscopy.
X-ray detection and recording
The x-ray image formed by the interaction of the x-ray beam and the patient must be detected and transformed into a visible format. The Image Intensifier captures the modulated x-ray beam emerging from the patient and converts it into a visible light to be viewed on an output screen. Image intensifiers are equipped with various sized image fields that alter the image resolution. The smaller the input screen diameter, the smaller the image field size and the sharper the resolution.
To obtain optimal cineangiograms, clinicians should be aware of the following principles:
- The image intensifier should be as close to the patient's chest as possible. This position optimizes the image detail and decreases scatter radiaition.
- The patient should be instructed to take a deep breath and hold it before the start of cineangiography. This pulls the diaphragm downward and out of the field of view.
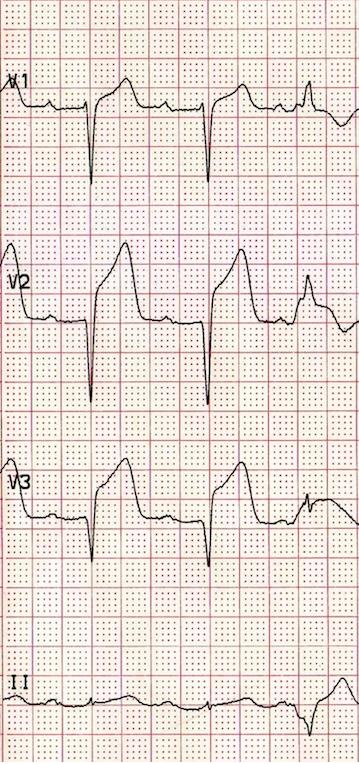
- All ECG electrodes, lead wires, metal snaps on the patient's gown, and jewelry should be out of the field of view before the start of the procedure. Keep wires and IV lines from hanging down under the table to prevent interference with the x-ray tube that may result in wires or lines from being pulled out.
- Use of collimators (shutters) eliminates unwanted lung field brightness and helps optimize exposure settings.
Radiation Safety
Four principles in radiation safety should be self-evident:
- The less exposure, the less chance of absorbed energy interaction.
- No known level of ionizing radiation is a permissible dose or absolutely safe.
- Radiation exposure is cumulative. No washout phenomenon occurs.
- Clinicians are obliged to minimize and reduce risks to other personnel and themseves
Methods to limit exposure
- Wear lead aprons: 0.5 mm or more thickness provides 80% protection
- Limit the fluoroscopic or cineagiographic time.
- Use collimators
- Reduce the distance between the x-ray source and the patient
- Maximize the distance between x-ray source and the operator and assistants
- Limit the milliamperes per kilovolts as much as possible for an adequate image.
- Use slower panning, and provide good intial angiographic setup. Angled views almost double the radiation
- Keep the image intensifier as low as possible
- Use extra shielding (thyroid, glasses, table shields)
References
- Baim, D.S. (2005) Grossman's Cardiac Catheterization, Angiography, and Intervention. (7th ed.). Philadelphia,Pa: Lippincott, Williams & Wilkins.
- Kern, M. et al (2003) The Cardiac Catheterization Handbook (4th ed.). Philadelphia, Pa: Mosby.