Left Ventricle Assessment
Regional LV Wall motion
- Hypokinesia refers to decreased motion or contraction of the heart muscle.
- Akinesia refers to paralysis of failure of part of the heart muscle during systole.
- Dyskinesia refers to an abnormal movement, usually outward, of the heart muscle during systole.

A point system is used to produce a wall motion score that reflects overall LV function. Points are assigned as follows:
- 1 = normal
- 2 = moderate hypokinesis
- 3 = severe hypokinesis
- 4 = akinesis
- 5 = dyskinesis
When each segment is scored and added together, a normal score = 5. Higher scores indicate more severe wall motion abnormalities.
Measuring Mitral Regurgitation
Mitral regurgitation is leakage of blood backward through an incompetent mitral valve each time the left ventricle contracts. As the left ventricle pumps blood into the aorta, some blood leaks backward into the left atrium, increasing blood volume and pressure there. The increased blood pressure in the left atrium increases blood pressure in the pulmonary veins and causes the left atrium to enlarge to accommodate the extra blood leaking back from the ventricle. Severe regurgitation can result in heart failure, in which increased pressure in the atrium causes fluid accumulation (congestion) in the lungs. The left ventricle may gradually enlarge and weaken, further worsening heart failure.
Angiographic grading:
1+ - contrast refluxes into the left atrium but clears with each beat
2+ - left atrial contrast density gradually increases but never equals left ventricular density
3+ - left atrial contrast density becomes equal to left ventricular density after several beats
4+ - left atrial contrast density is as dense as the left ventricle with contrast refluxing into the pulmonary veins

Hemodynamic assessment
While the catheter is in the Left Ventricle, hemodyamic information can be analyzed. Notice the wider pulse pressure of the Left Ventricle compared to the Aorta. During Isovlumetric contraction, the pressure in the ventricle rapidly rises. During the Isovolumetric relaxation phase, the pressure inside the ventricle rapidly falls.
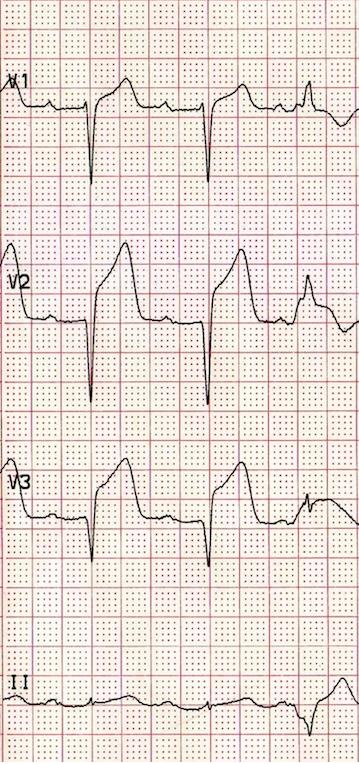
One of the most important measurements obtained from the LV waveform is Left Ventricular End Diastolic Pressure (LVEDP). This measurement is an indication of the preload, or volume of blood when the ventricle is maximally streched prior to contraction. Preload can indicate the functioning state of the Left Ventricle as it is one key factor in cardiac output. The LVEDP can be measured on the waveform at end diastole. A line drawn down from the R of the QRS to the LV waveform will give you the measurement of LVEDP. Normal range for LVEDP is 6 - 12 mmHg. An elevated LVEDP indicates a failing Left Ventricle and an inability to efficiently pump blood out of the chamber during systole. A decreased LVEDP can indicate a hypovolemic state.
The LV pressure should be initially measured at 200 scale with a normal sweep speed of 25 mm/second. A second measurement should be taken at 40 scale and a faster sweep speed of 50 - 100 mm/second. A faster sweep speed allows for greater analysis of the waveform. Finally the last measurement is taken as the catheter is pulled back from Left Ventricle to Aorta with 200 scale at normal sweep speed. (These images have shortened the scale to provide optimal viewing of the waveform)
The second most important measurement obtained from the LV waveform is measuring the comparison of the systolic pressure of the Left Ventricle and the systolic pressure of the Aorta. These pressures should be near identicle. A difference in systolic pressures (notably a higher LV systolic pressure than Aortic systolic pressure) indicates an abnormality of the Aortic Valve known as Aortic Stenosis. A stenotic, stiff, aortic valve requires the Left Ventricle to create a higher than normal pressure in order for blood to escape from the Left Ventricle and into the Aorta.
References
- Baim, D.S. (2005) Grossman's Cardiac Catheterization, Angiography, and Intervention. (7th ed.). Philadelphia,Pa: Lippincott, Williams & Wilkins.
- Kern, M. et al (2003) The Cardiac Catheterization Handbook (4th ed.). Philadelphia, Pa: Mosby.